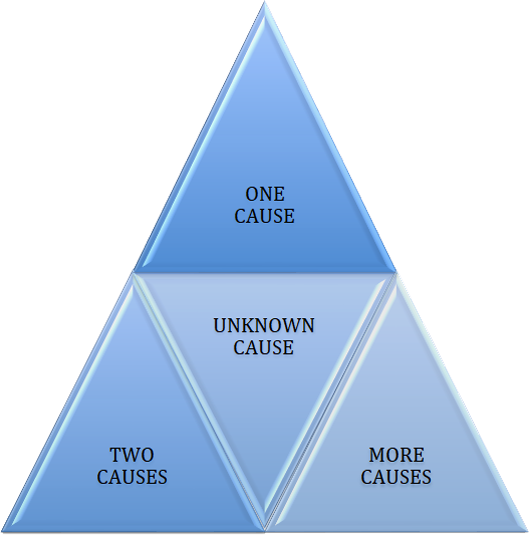
“Internal” causes

30% Unknown (idiopathic): likely to be a combination of genetic causes and environmental adverse effects.

Hormonal causes: the most common cause is reduced testosterone production in testicles by Leydig cells, i.e. hypogonadism. They may result from damaged testicles or deficiency of gonadotropins, mainly lutropin (LH) produced by the pituitary gland. Other causes include elevated corticosteroid levels (e.g. in Cushing’s disease), thyroid dysfunction, elevated levels of prolactin or estradiol.

Genetic causes: fertility processes are coded by about 1500 genes. The most important are located on Y chromosome in AZF region. We can also examine the genes responsible for the development of vas deferens (CFTR), as well as the system of all chromosomes, the so-called karyotype. The normal male karyotype is 46XY. A common genetic defect in the karyotype is Klinefelter syndrome.

Varicocele: it is the cause of 30% of primary infertility (inability to have the first pregnancy/child), and 85% of secondary infertility (problems occurred during attempts to have another child). This disease is congenital and progresses with the age of the patient. It may cause ailments such as pain or reduced testosterone levels.

Systemic causes: chronic diseases, as well as medication often taken in this regard, reduce fertility in various mechanisms. These include chronic kidney and liver failure, diabetes, severe neurological disorders.

Cryptorchidism, i.e. undescended testicles: in fetal life the testicles “descend” from the kidneys area to scrotum. If something disturbs this process and the testicles do not reach the scrotum, we are talking about cryptorchidism. Until the end of the first year of life in case of cryptorchidism, the testes should be brought down to the scrotum surgically.

Inflammation causes: inflammation of the prostate gland and epididymis may cause obstruction of the seminal tract, e.g. epididymis or ejaculation ducts. Chronic inflammation, also asymptomatic, may cause decreased mobility, total number and number of normal spermatozoa.

Erectile dysfunction and ejaculation: may hinder or prevent semen from entering the reproductive tract of a woman.

Immunological causes: the presence of anti-sperm antibodies may cause a decrease or lack of sperm motility.

Testicular tumors: both the testicular cancer and its treatment (surgery, chemotherapy or radiotherapy) cause a decrease in fertility.

Age: after 40 years of age, a man’s sperm parameters decrease.

Seed pathway obstruction: can be located at the intranuclear, epididymal (most common), vas deferens or ejaculatory ducts level. Its causes may be congenital/genetic (e.g. CFTR mutations), inflammatory, traumatic or iatrogenic (e.g. vasectomy).
“External” causes
which is an unfavorable lifestyle and environmental pollution

Obesity: reduces fertility in many mechanisms, including: decreased testosterone level, elevated estradiol level, erectile dysfunction.

Environmental contamination: hundreds of substances present in soil, air, water and food cause damage to spermatogenesis. Industrial pollution of the environment is attributed to constant reduction of semen parameters in recent decades. Oil processing products are particularly burdensome.

Medicines, stimulants, household chemistry: from anabolic steroids, through tobacco, alcohol and drugs to ubiquitous softeners / plasticizers – all these substances have an adverse effect on sperm production.

Lifestyle: stress, lack of exercise/moderate physical activity, sedentary lifestyle and work, diet (the best is Mediterranean), overheating of testicles: hot baths / sauna.

Occupational exposure: high temperatures, X-rays, electromagnetic radiation, WiFi, mobile phones, chemical vapors.
Diagnostics
The basic test in diagnosis of male fertility is semen analysis.
- Computer semen analysis (CASA), determining the physicochemical parameters of semen: volume of ejaculate, viscosity, liquefaction, concentration and number of sperm, their motility, percentage of live cells, survival rate and number of properly formed cells, as well as the presence of other cells (e.g. responsible for inflammation of leukocytes).
- DNA fragmentation test. Various types of research on the correct ordering of sperm genetic material. In general, a result of more than 25-30% of defragmented sperm is considered abnormal. Based on this single numerical parameter, it can be concluded whether natural fertilization is possible, difficult or impossible.
- Specialized tests: functional (e.g. MAR test, hyaluronic acid binding test, swim-up test) and biochemical (e.g. determination of citric acid, fructose, neutral glucosidase NAG), reflect the state of prostate function (prostate gland), seminal vesicles and epididymis.
- Scrotum organ ultrasound with Color Doppler vascular flow evaluation: allows to confirm the diagnosis of clinically significant varicose veins of seminal cordage, diagnosis of neoplasms and micro-dilutions of testicles, as well as other pathologies: epididymal cyst/seed cyst, hydrocele testis.
- Hormonal tests: testosterone, sex hormone-binding globulin, lutropin, follicle stimulating hormone, prolactin, estradiol, cortisol, thyrotropin and markers of testicular tumors: alpha-fetoprotein and beta HCG.
- Genetic tests: karyotype, AZF microdeletions, CFTR mutations are performed in cases of lack of sperm (azoospermia), their very low concentration (<million/ml) or lack of mobility.
Semen analysis – spermogram, CASA
Based on the spermiogram, we can conclude that male fertility is normal or reduced. In the medical nomenclature, based on WHO guidelines published in 2010, we use the following terms:
- Oligozoospermia: reduced concentration (<million/ml) and/or total sperm count (<39 million./ejaculate).
- Hypospermia: reduced volume of ejaculate (<1,5ml).
- Astenozoospermia: reduced sperm motility (progressive motion <32% and/or total motion <40%).
- Teratozoospermia: reduced percentage of normal sperm (<4%).
- Azoospermia: no sperm in the ejaculate.
- Cryptospermia: single sperm in the field of vision.
- Leukospermia: increased leukocyte count (white blood cells) in the ejaculate (>million/ml).